HPV Vaccine – Need, Risk, and Benefits!
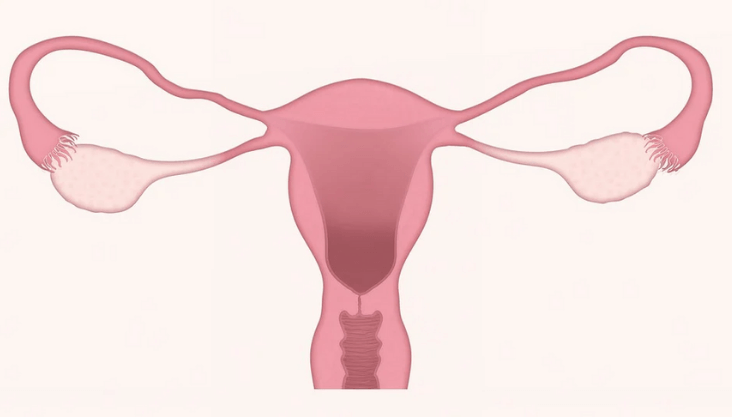
HPV vaccines are human papillomavirus vaccines that protect against infection. HPV is a class of more than 200 associated viruses, more than 40 of which are transmitted through personal sexual activity. Two types of HPV cause genital warts among these, and around a dozen types of HPV may cause some forms of cervical, anal, oropharyngeal, penile, vulvar, and vaginal cancer.
Who can get the HPV vaccine?
Vaccination against HPV is typically prescribed at age 11 or 12; vaccination can begin as early as age 9. Immunization against HPV is prescribed for all individuals over the age of 26 who have not been sufficiently vaccinated before.
Even though the HPV vaccine is approved by the Food and Drug Administration to be administered through age 45, vaccination with HPV is not recommended for all adults aged 27 to 45. Instead, the Advisory Committee on Immunization Practices recommends that clinicians recognize addressing whether HPV vaccination is right for them with their patients in this age group who were not adequately vaccinated earlier.
HPV vaccination must be deferred till after pregnancy but pregnancy testing before vaccination also isn’t required. There is no evidence to indicate that vaccination impacts a pregnancy or damages a fetus.
Ways HPV vaccines work
Like many vaccinations that protect from viral infections, HPV vaccines enable the body to develop antibodies that attach to the virus and stop it from infecting cells in future contact with HPV.
The latest HPV vaccines are centered on virus-like particles produced from elements of the HPV surface. VLPs do not become contagious since they lack the DNA of the virus.
They strongly match the real virus, nevertheless, and antibodies to the VLPs still work against the real virus. The VLPs were shown to be highly immunogenic, implying they cause the body to produce elevated amounts of antibody production. But the vaccines are incredibly successful.
The vaccines neither prevent other sexually transmitted diseases nor treat existing HPV infections
How successful are vaccines against HPV?
HPV vaccines are extremely effective in avoiding infection with the forms of HPV that they target when administered before actual exposure to the disease, meaning before individuals initiate sexual activity.
In the studies that contributed to the authorization of Gardasil and Cervarix, these shots have been found to provide nearly complete protection against recurrent HPV types 16 and 18 in cervical infections.
Gardasil 9 is as useful in preventing diseases caused by the four HPV types 6, 11, 16, and 18, focused on identical antibody responses in clinical trial participants. The studies that led to Gardasil 9 ‘s support reported it to be almost 100% helpful in the reduction of cervical, vulvar and vaginal illnesses transmitted by the five HPV forms 31, 33, 45, 52, and 58.
Why is it essential for humans to adopt guidelines for HPV vaccination?
The mix of the HPV vaccine and cervical screening would provide the highest degree of cervical cancer safety. Vaccination is also the licensed public health measure intended to minimize the chance of developing HPV-related cancers at locations besides the cervix.
Many people must get vaccinated in the appropriate age group. Vaccination not only prevents vaccinated individuals from infection by the HPV types targeted by the specific vaccine but even vaccination of a large chunk of the population will reduce the occurrence of vaccine-targeted HPV types in the population and also provide some security.
Prevalent HPV vaccination will reduce the risk of cervical cancer by as much as 90 percent across the world. Furthermore, the vaccines could reduce any need for screening and associated medical treatment, biopsies, and invasive procedures connected with follow-up from irregular cervical screening, thereby helping to reduce the cost of healthcare and the anxieties involved with follow-up.
The other cancers caused by HPV have until recently been less common than cervical cancer. Even so, the occurrence has increased in HPV-positive oropharyngeal cancer and anal cancer. Moreover, most of the non-cervical HPV-positive cancers occur in men. For non-cervical cancers, there are no established screening services, so compulsory vaccination may have a major public health impact.
What is the efficacy of HPV vaccines?
All three HPV vaccines had been tested for efficacy and safety in thousands of people in the United States and several other countries before they could be approved. Millions of people were vaccinated since approval, so far no severe side effects are triggered by the shots. Brief soreness or other local symptoms are perhaps the most common issues.
A safety analysis by the FDA and the CDC deemed serious Gardasil immunization-related side effects that have been recorded to the Vaccine Adverse Events Monitoring System since the vaccine was approved. The rates of negative side effects in the safety analysis were compatible with the safety studies performed before authorization of the vaccine and were close to those seen with other vaccines.
Even so, Gardasil has had a greater proportion of dizziness and blood clots than is commonly associated with other shots. The patients who formed blood clots had recognized risk factors such as using oral contraceptives to develop them.
Gardasil has had a larger percentage of fainting and blood clots than is normally seen with many other vaccinations. Patients who developed blood clots, such as taking oral contraceptives, have a known probability of developing them.
Can HPV vaccines be administered to women who already are HPV infected or who have cervical cell changes?
ACIP suggests that women with an HPV infection or an irregular Pap test result that may suggest an HPV infection still should receive HPV vaccination if they are in the suitable age group so the shot may shield them from the high-risk HPV forms that they’ve not contracted. These women should nevertheless be advised that the vaccine would not cure them of existing HPV infections.
While HPV vaccines are effective when administered to people previously infected with HPV, the vaccines may not treat the infection. They offer a maximum advantage if they are obtained by an individual before he or she is sexually active.
Would women who’ve been vaccinated still need cervical cancer screening?
Since HPV vaccinations may not protect against all forms of HPV which may lead to cancer, it is estimated that patients who have been vaccinated follow the very same screening guidelines as women who are not vaccinated. Recent screening guidelines for women who have been vaccinated may change.
Are you concerned with your vaginal health? Want to know more about women’s health please connect with our specialists today.